Parasite Medical Program
As many as 300,000 Tibetan herders (nomads) are suffering from a deadly parasitic disease called echinococcosis. It progresses through early stages unknown to the infected person, unless detected by medical tests. If not treated, this widespread disease can cause failure of the liver or lungs, which leads to a painful death. Tibetan children, adults, and monks become infected through poor sanitation and contact with infected dogs.
In Summer 1997, Carol Delker, BLSCP member, assisted a renowned medical research team for several weeks in remote Tibetan villages in northwest Sichuan and southeast Qinghai. Centers for Disease Control and Prevention (CDC), Atlanta, Georgia was the lead institution. A total of 7,702 Tibetans were tested for this disease. The average infection rate was measured to be 5.6%. A summary of the research is provided in Echinococcosis on the Tibetan Plateau: Risk Factors for Infection in Tibetan Populations, by Dr. Peter M. Schantz. Click here to view a pictorial diagram of the life cycle of the parasite that causes echinococcosis. | |
|---|---|
 | |
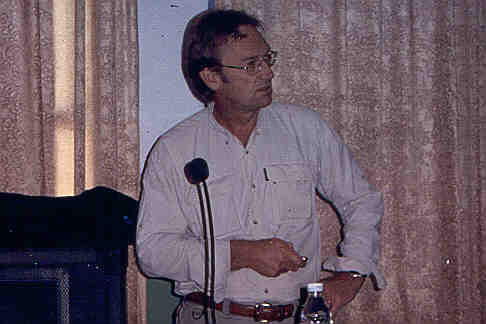 |
In September 2002, Bill Warnock, BLSCP member, led an information exchange with Lhasa City Hospital
on echinococcosis. The other BLSCP delegate was Prof. Philip S. Craig, University of Salford, United Kingdom, a renowned expert on the disease. In this photo, Prof. Craig delivers a lecture on the disease to the medical staff of Lhasa City Hospital. They discussed the disease with many health care personnel at city, county, and village levels. In cooperation with Lhasa City Hospital, they developed a long-term plan for training on diagnosis and treatment, as well as control and prevention. This exchange was funded through many individual and corporate donations.
|
 | |
|
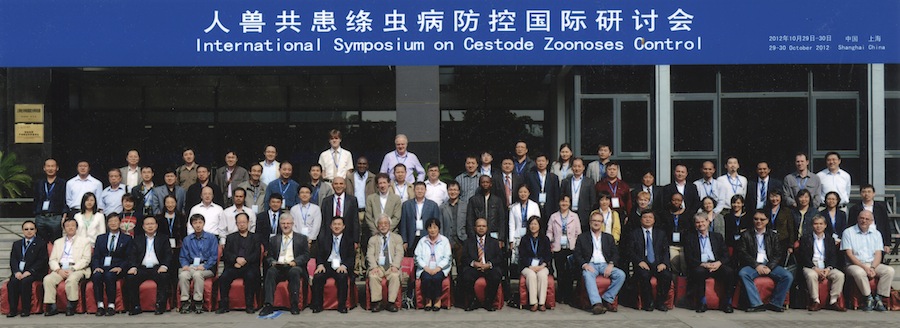
In May 2006, Bill Warnock, BLSCP member, attended an International Workshop on "Treatment,
Prevention and Control of Echinococcosis" in Chengdu, Sichuan, China, which was hosted by Sichuan Center for Disease Control and Prevention. The 70 workshop participants, shown in this photo, were from China and eight foreign countries. The purpose of the workshop was to provide a regional, national, and international platform to consider the public health impact of echinococcosis, to consider optimization and improvement in treatment of human cases, to discuss risk factors, epidemiology and transmission, and assess the potential for current and long-term future control strategies in Tibetan community areas. BLSCP networked with many stakeholders about the need for a training project on diagnosis and treatment of echinococcosis with Lhasa City Hospital and developed new strategies for implementing the training project. Workshop participation and support was funded by a $5,000 grant
from the Everest '96 Memorial Fund
of The Community Foundation Serving Boulder County.
 In September 2010, BLSCP members Bill Warnock, Carol Delker (registered nurse), and Megan Newton (professional photographer) led a 7-day training exchange in Lhasa Prefecture with Lhasa Municipal Health Bureau on "Diagnosis and Treatment of Echinococcosis." BLSCP's five expert trainers provided several lectures and demonstrations regarding this deadly parasite disease, which is causing extensive suffering by rural Tibetans. Click here to view a summary of the training exchange with several photos (PDF). In October 2012, Bill Warnock, BLSCP member, attended an International Symposium on Cestode Zoonoses Control in Shanghai, China. Cestode zoonoses are tapeworm diseases that can be passed from animals, whether wild or domesticated, to humans. The symposium was organized by National Institute of Parasitic Diseases (Chinese Center for Disease Control and Prevention) and Asahikawa Medical University, Japan. With travel expenses paid from Bill's personal funds, he attended the symposium and made a presentation on "Echinococcosis Training in Tibet", which describes the BLSCP training exchange in Lhasa during September 2010. The symposium was attended by 96 participants from 13 countries, Chinese Ministry of Health, and World Health Organization. Bill was the only participant from the U.S.A.
 Cestode zoonoses are a group of diseases being neglected by the global health community but causing serious health and economic damage to humans and livestock. Global control activities are still insufficient, particularly in Asian countries. The Shanghai symposium was organized to promote further global collective efforts and action for cestode zoonoses control. A total of 39 speakers addressed cestode zoonoses with respect to the current global situation, the status in Asian countries, and recent progress in Asia on epidemiology, ecology, biology, immunology, molecular taxonomy and phylogeny, control strategy, diagnosis, vaccine research, clinical treatment, and public policy related to control. Most of the presentations were on echinococcosis and taeniasis/cysticercosis in Asia. After the presentations, all participants engaged in a round-table discussion on how to make a systematic assessment of the current epidemic status of cestode zoonoses and control strategy for cestode zoonoses. For the epidemiology and control of echinococcosis and taeniasis/cysticercosis, several "gaps" (missing elements in ongoing work) were identified. One of the gaps for control is "health education", i.e., education of communities where these diseases are prevalent. Education topics include life cycle of the parasite, how humans are infected, prevention methods, and control strategies. | |
 | |
|
Dr. Li Tiaoying, Sichuan Institute of Parasitic Diseases, made a presentation on "Current status of taeniasis/cysticercosis in Tibetan communities of Sichuan Province, China". Humans are infected with taeniasis by eating raw or undercooked infected meat from pigs or cattle/yak. This can lead to adult tapeworms in the small intestine. Humans are infected with cysticercosis through fecal-oral contamination from (human) tapeworm carriers. Human cysticercosis can lead to cysts (cysticerci) in the brain or eyes, which can cause epileptic seizures or blindness, respectively. The taeniasis infection rate of Tibetan farmers in 11 villages of Yajiang County in western Sichuan Province (Kham) was measured to be 21%. The prevalence of human cysticercosis in these villages was measured to be 7%. Risk factors include a high proportion of consumption of raw beef and/or undercooked beef/pork, the use of free-ranging pigs and yak, lack of latrine facilities, lack of meat inspection, poor hygiene, and a poor economy. A pictorial diagram of the life cycle of the parasite that causes taeniasis/cysticercosis shows how this parasite can cause human cysticercosis. Click here to view Dr. Li's presentation (PDF).
|
 |
 | |
 |
On slide #11 of Dr. Li’s presentation, “Seroprevalence of cysticercosis in Tibetan populations of Yajiang,” she shows a photo of a teen-age Tibetan girl from Weidi village for whom the cysticercosis caused total blindness in both eyes. BLSCP decided to raise funds to help this girl, Lhungtse, receive the brain surgery that was indicated for her disease. BLSCP member Bill Warnock and Dr. Li worked together to coordinate the details of the surgery. During August-September 2013, Bill spent a month with Lhungtse and her mother to arrange and manage the surgery. During August, she was evaluated by neurosurgeons at Huaxi Hospital in Chengdu, Sichuan, and at Dali University Hospital in Dali, Yunnan. On September 5, ventriculoperitoneal (VP) shunt brain surgery was performed successfully at Sichuan Provincial People’s Hospital in Chengdu. In this photo, Dr. Li is talking with Lhungtse in Chengdu in early October 2013. On the previous day, Lhungtse had successfully completed her first post-surgery check-up at Sichuan Provincial People’s Hospital. Click here to view our report on Lhungtse's surgery with 8 photos (PDF).
|
 | |
|
Lhungtse returned to the Neurosurgery Department of Sichuan Provincial People's Hospital (SPPH) in Chengdu for additional check-ups in January and July 2014. The MRI image of her brain in July 2014 showed that the ventricles had returned to normal size and that her three two-week courses of albendazole had killed the active parasitic cysts. However, the MRI image also showed that some calcified lesions had occurred in the brain parenchyma, which can cause epileptic seizures. On 4 February 2015, Lhungtse completed her fourth periodic check-up at SPPH. On 9 February 2015, Lhungtse was examined by Dr. Zeng Xian Rong, a neurologist in Chengdu, and given an electroencephalogram (EEG) test, as shown in this photo. Some abnormalities apparently caused by calcified lesions were found, and she was given an anti-epilepsy drug called oxcarbazepine. In late April-early May 2015, BLSCP members Bill Warnock and Shari Mayer traveled to Sichuan Province to visit Lhungtse and two of her doctors. Click here to view our trip report with 6 photos (PDF). In November 2015, Bill and Shari traveled again to Sichuan Province to visit Lhungtse, two of her doctors, and several others. Click here to view our trip report with 4 photos (PDF). In late October-early November 2016, Bill and Shari traveled to Chengdu, Sichuan, to take Lhungtse to her neurologist for an examination and tests. Click here to view our trip report with 4 photos (PDF).
|
 |
 | |
 |
On 21 October 2017, BLSCP conducted the Shuiluo Student MRI Project in Xichang, Sichuan. MRI brain scans performed for 44 students and 3 adults revealed 11 cases of neurocysticercosis. Dr. Li Tiaoying hopes that 10 of these patients can be cured with appropriate drug therapy. The other patient is Lhosang Drolkar (shown here in December 2016), a 19-year-old Tibetan woman from Muli County, Donglang Township, whose MRI showed many cysts and severe hydrocephalus. Her symptoms indicated an urgent need for brain surgery. BLSCP contributed a Shuiluo Student MRI Project surplus of $9,707 as a major percentage of the cost of this surgery, which was successfully performed in Chengdu on November 6. Click here to view our trip report with 15 photos (PDF).
|
 | |
|
On 4-6 September 2018, in collaboration with Dr. Li Tiaoying, Sichuan CDC, we conducted a 3-day pilot training project for rural Tibetan doctors in Shuiluo Township, Muli County, on prevention of neurocysticercosis (NCC). NCC is a dangerous parasitic disease that is highly prevalent in 24 counties in western and southern Sichuan Province of China (Kham). Click here to view our report on this work, with 7 photos and cost data.
| |
 | |
|
On 22-30 October 2018, BLSCP members Bill Warnock and Shari Mayer were joined by Aaron Miller (Bill’s nephew) on a trip to Chengdu and Kham to spend time with Lhungtse and her mother. After we learned in 2017 that Lhungtse loves the piano, Bill invited Aaron to join us on this trip and offer keyboard lessons to Lhungtse. Aaron is a full-time keyboard instructor in Bend, Oregon. Click here to view our report on this work, with 5 photos and cost data.
| |
 | |
|
In late October 2019, BLSCP member Bill Warnock traveled to Chengdu to spend several days with Lhungtse and her mother. We arranged for Lhungtse her annual medical checkup and a keyboard lesson. Click here to view our report on this work, with 4 photos and cost data.
| |
 | |
|
Taeniasis refers to the parasitic infection of adult stages (tapeworms) of three Taenia species. Roundworm and whipworm are soil-transmitted parasitic infections. These five parasitic diseases are highly prevalent in southwestern Muli County, Sichuan Province, China (Kham). During June-December 2019, our partner, Dr. Li Tiaoying, Sichuan CDC, Chengdu, worked to eliminate these five diseases in 535 Tibetan children attending two primary schools in Muli County. Click here to view final results for this project.
| |
 | |
|
On 7-13 October 2020, Tenpa drove Lhungtse & her mother to Chengdu, managed Lhungtse’s medical checkup, bought medicine, and returned them to their home in Kham. To view our report, including photos and a cost breakdown, click here.
| |
 | |
|
On 12-13 May 2021, Dr. Li Tiaoying, Sichuan CDC, and Dr. Duan Mian Chuan, Muli County CDC, trained 340 Yiji Primary School students (1st-6th grade), 13 homeroom teachers, and 30 Yiji Township medical staff members and village cadres (government workers) on taeniasis and neurocysticercosis (NCC). To view our report, including photos and a cost breakdown, click here.
| |
 | |
|
On 17-26 October 2021, Tenpa drove Lhungtse & her mother to Chengdu, managed Lhungtse’s annual medical checkup, bought medicine, and returned them to their home in Kham. To view our report, including photos and a cost breakdown, click here.
| |
 | |
|
On 1-5 November 2022, Tenpa drove Lhungtse & her mother to Chengdu, managed Lhungtse’s medical checkup, bought medicine, and returned them to their home in Kham. To view our report, including photos and a cost breakdown, click here.
| |
 | |
|
During 2022, Dr. Li Tiaoying, Sichuan CDC, Chengdu, and her team trained rural doctors in Muli County, Sichuan Province (Kham) on (1) all aspects of taeniasis and neurocysticercosis (NCC), (2) how to identify taeniasis carriers, (3) how to conduct treatment, including preparation of the herbal medicines, and (4) how to record the results of treatment. To view our final report, click here.
| |
 | |
|
On 26-30 October 2023, Tenpa drove Lhungtse & her mother to Chengdu, managed Lhungtse’s medical checkup, bought medicine, and returned them to their home in Kham. To view our report, including photos and a cost breakdown, click here.
| |
 | |
|
Based upon the success of our 2022 project, the Sichuan Provincial Finance Department for Public Health has appropriated 5 RMB per each Muli County resident to be used in 2023 by rural doctors in the county for the detection and treatment of taeniasis. With the Muli County population being 130,000, the total amount is 650,000 RMB (~100,000 USD). To optimize the use of the 650,000 RMB, more rural doctors needed to be trained to treat taeniasis carriers with the herbal medicines. BLSCP collaborated with Dr. Li Tiaoying, Sichuan CDC, for a 2023 project to extend our 2022 taeniasis training model to four additional townships in Muli County with high taeniasis infection rates. This project was successfully conducted in mid-April 2023. To view a project description, click here.
| |
 | |
|
On 14-18 November 2024, Tenpa drove Lhungtse, her mother, & her brother to Chengdu, managed Lhungtse’s medical checkup, bought medicine, and returned them to their home in Kham. To view our report, including photos and a cost breakdown, click here.
| |
| Contact: | Bill Warnock |
|---|---|
| Phone: | 303-443-9863 |
| E-mail: | health@boulder-tibet.org |